How AI-Powered Teleradiology Transforms Oncology and Cancer Care?
Faster Cancer Diagnosis, Better Patient Care
Written by: Mohamed Hammam, Medical Liaison at Rology

Cancer is a large and growing global health concern, with 18.1 million new cancer cases and 9.6 million cancer deaths estimated to have occurred globally in 2018 [1], and the burden is projected to increase by more than 20% in 2030 to 22 million cases and 11.7 million deaths [2]. This burden falls disproportionately on low-income and middle-income countries (LMICs), which account for approximately 80% of disability-adjusted life years lost to cancer. Still, only 5% of global resources are spent on cancer care [3]. In recent years, the demand for precise, timely, and accessible diagnostic imaging in oncology has surged, driven by the rising global cancer burden [4].
Oncology diagnosis, often reliant on advanced imaging modalities like CT scans, MRIs, and mammograms, plays a critical role in early detection, staging, and monitoring of cancer progression. However, a shortage of radiologists, particularly in remote and underserved regions, poses a significant challenge to delivering optimal care. This gap is bridged by teleradiology, a technology-driven solution that enables radiologists to remotely interpret and report imaging studies [5, 6].
Teleradiology integrates cutting-edge imaging technologies, high-speed data transfer, and artificial intelligence (AI) to revolutionize oncology care. Overcoming geographical and logistical barriers ensures timely diagnosis and intervention, improving patient outcomes [4, 7]. In this article, we explore the growing market for teleradiology, its significance in oncology cases, and its potential to transform cancer care. Furthermore, we delve into the significant contributions of Rology, an AI-powered teleradiology platform, showcasing its contributions in streamlining diagnostics, reducing reporting delays, and ensuring timely intervention in cancer care in underserved areas.
Teleradiology & AI: Transforming Cancer Diagnosis Worldwide
Teleradiology has emerged as a key component of the global medical imaging market, with significant growth attributed to its ability to address radiologist shortages and streamline diagnostic workflows. Recent studies underscore its critical impact. For instance, teleradiology consultations have been shown to alter cancer diagnoses in up to 62% of cases, thereby significantly influencing treatment decisions in resource-limited settings [8]. The global teleradiology market is projected to grow at a compound annual growth rate (CAGR) of 18.5% in 2024, driven by increased adoption of AI-based imaging solutions and rising healthcare demands in developing regions [9]. Moreover, teleradiology has demonstrated exceptional utility in emergency settings, achieving an average turnaround time of 35 minutes for ultrasound reports, even during peak periods [10].
In oncology, teleradiology is transformative by enabling high-quality diagnostics in underserved areas. For instance, during the COVID-19 pandemic, teleradiology networks demonstrated resilience and capacity by adapting to a surge in demand for radiological interpretations, including oncological imaging [11]. Additionally, its integration with artificial intelligence has further enhanced diagnostic accuracy and efficiency, enabling early detection of diseases and reducing diagnostic errors [12].
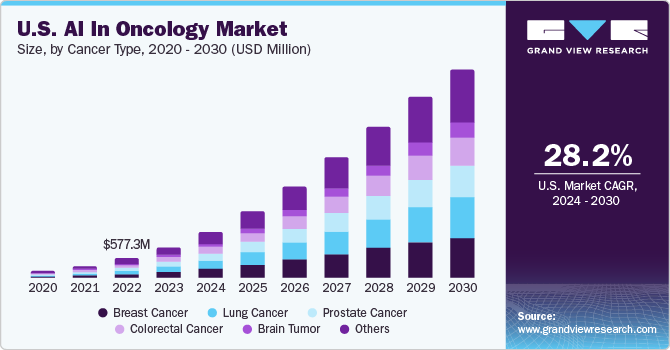
The Rapid Growth of AI in Oncology
The global AI in oncology market was valued at USD 2.80 billion in 2023 and is projected to expand at a CAGR of 28.92% from 2024 to 2030. This surge is fueled by the rising prevalence of cancer, advancements in diagnostic technology, and growing demand for early, precise cancer detection [15].
The Role of Teleradiology in Oncology
- Early Detection and Improved Diagnosis
Early detection is paramount in cancer care, significantly improving survival rates. Teleradiology ensures the availability of specialized expertise for accurate interpretation of imaging studies, even in remote locations. Mobile mammography units equipped with teleradiology systems have proven particularly effective, with one initiative in India reducing diagnostic turnaround times to an average of 12 hours for breast cancer detection [13].
- Follow-Up Scans and Longitudinal Monitoring
Oncology care often involves frequent imaging to assess treatment response and detect recurrence [14]. Teleradiology enables real-time comparisons with previous scans, ensuring precise monitoring over time. AI-powered platforms like rology further enhance this process by identifying subtle changes in tumor size or morphology, which may be missed by manual interpretation.
- Workflow Optimization and Cost Efficiency
Teleradiology platforms enhance diagnostic accuracy and streamline workflows by prioritizing urgent cases and reducing unnecessary interventions. A study revealed that teleradiology reduced exploratory surgery (72% decrease) and surgical orthopedic intervention (62% decrease) in resource-limited settings, allowing more conservative medical or surgical management and emphasizing its role in cost-effective cancer care [8].
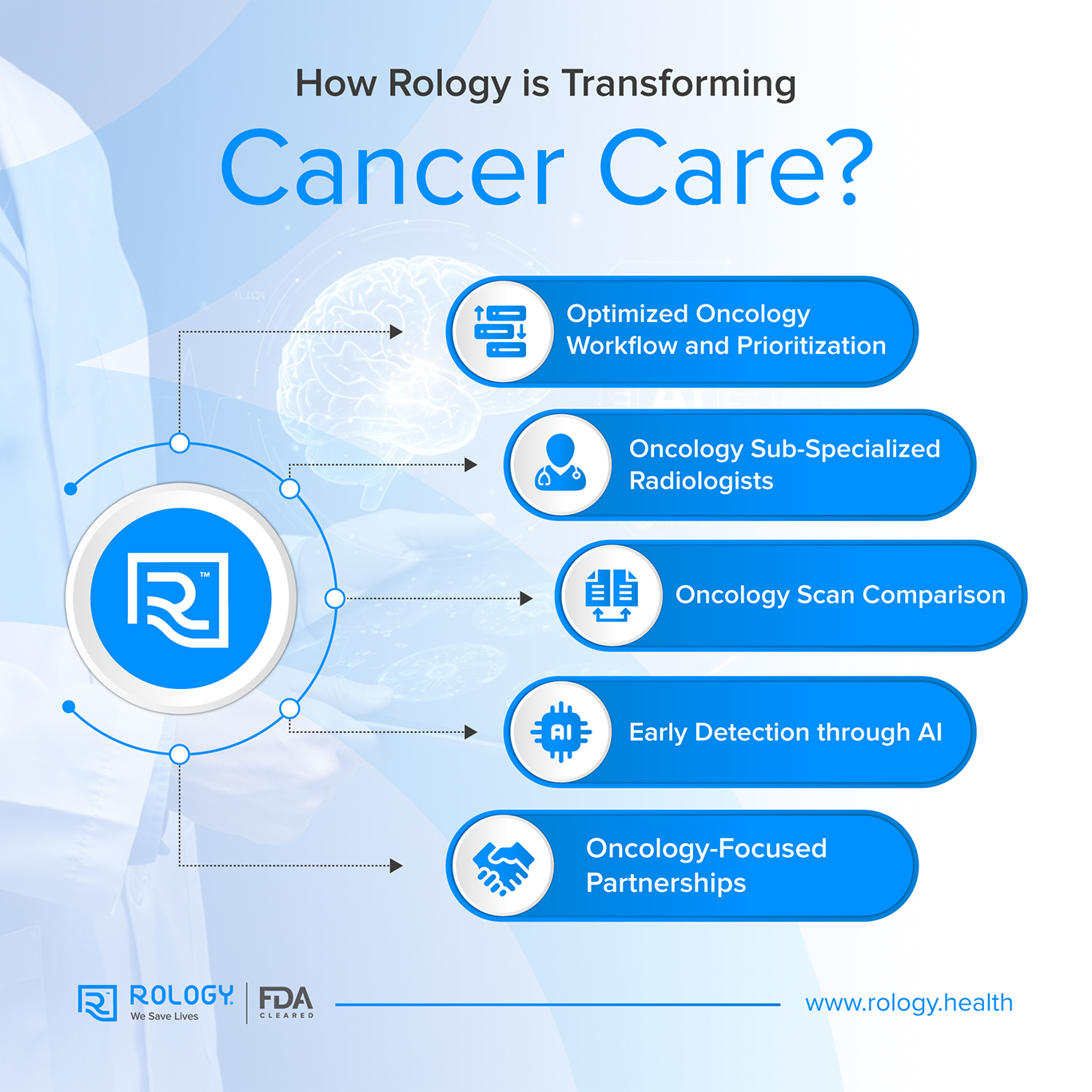
What Makes Rology’s AI-powered Teleradiology a Game-Changer in Oncology and Cancer Care?
Rology is at the forefront of teleradiology innovation, offering a comprehensive solution for modern oncology diagnostics. The integration of Rology has dramatically improved oncology workflows through:
- Optimized Oncology Workflow and Prioritization: The platform’s capabilities include prioritizing urgent and critical studies (e.g., oncology emergencies), ensuring fast turnaround times, and reducing diagnosis delays. This is particularly significant for life-threatening conditions like cancers.
- Oncology Sub-Specialized Radiologists: Oncology scans are matched with highly trained and sub-specialized radiologists in oncology to ensure accurate and timely diagnosis.
- Comprehensive Oncology Scan Comparison: Rology’s platform enables radiologists to compare current and past oncology scans, tracking tumor progression, treatment response, and subtle changes over time. This historical analysis ensures more accurate diagnoses and better-informed treatment decisions.
- Early Detection through AI: Rology’s AI assists in the detection of lung nodules as small as 5 mm, which may take a radiologist 1–2 minutes to detect manually and can often be missed. This automation significantly improves early detection rates, which is particularly crucial for early-stage lung cancer diagnosis.
- Oncology-Focused Partnerships: Rology has partnered with AstraZeneca to focus on the early diagnosis of lung cancer. This collaboration emphasizes the role of AI and early screening in combating oncology-related challenges. This should lead to class shifting for detection, increasing the curing rate, and reducing the overall healthcare cost.
Case Study: The Power of Rology
In an underserved oncology hospital, Rology transformed a slow and inefficient diagnostic workflow. Previously, MRI images had to be manually transferred onto external drives or USB flash memory and physically sent to external consultant radiologists for interpretation. The hospital also relied on on-site radiologists traveling from other cities, further delaying diagnoses. This time-consuming process compromised both report accuracy and quality, ultimately delaying critical patient care.
With 24/7 AI-powered teleradiology services, Rology revolutionized the center’s operations, drastically reducing turnaround times and improving diagnostic precision.
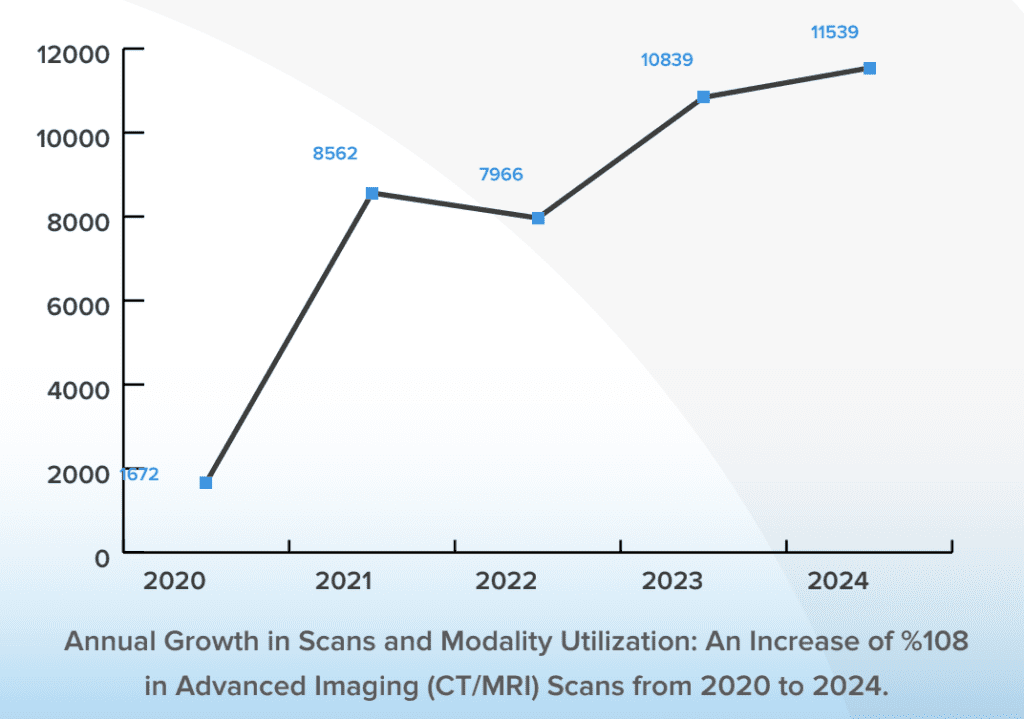
- Improved imaging utilization by 108%, increasing the number of CT/MRI scans (2020-2024) due to optimized workflows.
- Decreased emergency scan turnaround time to 60 minutes.
- Optimized the standard case time of diagnosis, which is now processed in a couple of hours instead of 10 days.
- Maintained an average of a 99.92% accuracy rate, minimizing errors and improving early cancer detection using Rology’s AI-powered system.
- Track the previous studies for comparison, allowing radiologists using Rology’s reporting system to easily compare new and previous imaging results for better treatment challenges
- Reduces diagnostic inconsistencies with AI-assisted peer-reviewed reports.
- Provide flexible payment solutions by adapting to customized-reimbursed hospitals.
- Provides round-the-clock 7/24 technical assistance and comprehensive customer success support, promptly resolving any issues that could disrupt radiology services.
This real-world evidence underscores how teleradiology can bridge healthcare gaps, ensuring faster, more accurate cancer diagnoses.
Conclusion
Teleradiology is a transformative tool in oncology, bridging gaps in access, expertise, and efficiency. Platforms like Rology exemplify how AI-driven solutions can revolutionize cancer diagnostics, ensuring better patient outcomes worldwide. The success of Rology integration with the public oncology center proves that teleradiology is not just an emerging technology; it’s a necessity. Healthcare providers, especially in low-resource settings, must integrate AI-driven solutions to enhance cancer care, reduce delays, and save lives. As the global demand for radiology services grows, teleradiology will remain essential in advancing oncology care.
If your healthcare facility is interested in leveraging Rology’s cutting-edge technology to streamline workflows and improve diagnostic accuracy, we invite you to learn more and contact us. Visit Rology website to explore how we can support your needs and help you achieve excellence in radiological services.
References:
1- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68(6): 394–424.
2- Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. Lancet Oncol 2012; 13(8): 790–801.
3- Farmer P, Frenk J, Knaul FM, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet 2010; 376(9747): 1186–93.
4- Ward, Z., Scott, A., Hricak, H., & Atun, R. (2021). Global costs, health benefits, and economic benefits of scaling up treatment and imaging modalities for survival of 11 cancers: a simulation-based analysis. The Lancet. Oncology, 22 3, 341-350 . https://doi.org/10.1016/S1470-2045(20)30750-6.
5- Hricak, H., Abdel-Wahab, M., Atun, R., Lette, M., Paez, D., Brink, J., Donoso-Bach, L., Frija, G., Hierath, M., Holmberg, O., Khong, P., Lewis, J., McGinty, G., Oyen, W., Shulman, L., Ward, Z., & Scott, A. (2021). Medical imaging and nuclear medicine: a Lancet Oncology Commission.. The Lancet. Oncology. https://doi.org/10.1016/S1470-2045(20)30751-8.
6- Daly, R., Brawley, O., Gospodarowicz, M., Olopade, O., Fashoyin, I., Smart, V., Chang, I., Tendler, C., Kim, G., Fuchs, C., Zhang, L., Legos, J., Durán, C., Kalidas, C., Qian, J., Finnegan, J., Pilarski, P., Silverstein, A., Wu, Y., & Li, B. (2023). Global adoption of remote technologies to enable patient-centric oncology clinical trials: Analysis by the Bloomberg New Economy International Cancer Coalition.. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2023.41.16_suppl.1584.
7- Cheung, H., & Rubin, D. (2021). Challenges and opportunities for artificial intelligence in oncological imaging.. Clinical radiology. https://doi.org/10.1016/j.crad.2021.03.009.
8- Crumley, I., Halton, J., Greig, J., Kahunga, L., Mwanga, J., Chua, A., & Kosack, C. (2020). The impact of computed radiography and teleradiology on patients’ diagnosis and treatment in Mweso, the Democratic Republic of Congo. PLoS ONE, 15. https://doi.org/10.1371/journal.pone.0227773.
9- Tele-Radiology Global Market Report 2025
10- Kalyanpur, A., & Mathur, N. (2024). The Role of Teleradiology in Interpretation of Ultrasounds Performed in the Emergency Setting. Digital Diagnostics. https://doi.org/10.17816/dd624586.
11- Vatele, J., Gentile, S., Thomson, V., Devictor, B., Cloux, M., Girouin, N., Bratan, F., Bergerot, J., Seux, M., Banaste, N., Tazarourte, K., & Gorincour, G. (2020). Teleradiology as a relevant indicator of the impact of COVID-19 pandemic management on emergency room activities: a nationwide worrisome survey. Insights into Imaging, 12. https://doi.org/10.1186/s13244-021-00964-0.
12- Daly, R., Brawley, O., Gospodarowicz, M., Olopade, O., Fashoyin, I., Smart, V., Chang, I., Tendler, C., Kim, G., Fuchs, C., Zhang, L., Legos, J., Durán, C., Kalidas, C., Qian, J., Finnegan, J., Pilarski, P., Silverstein, A., Wu, Y., & Li, B. (2023). Global adoption of remote technologies to enable patient-centric oncology clinical trials: Analysis by the Bloomberg New Economy International Cancer Coalition.. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2023.41.16_suppl.1584.
13- Kalyanpur, A., Sudhindra, R., & Rao, P. (2022). The Role of Mobile Van Mammography Supported by Teleradiology in the Early Diagnosis of Breast Cancer: An Innovative Approach to a Growing Public Health Problem. International Journal of Health Technology and Innovation. https://doi.org/10.60142/ijhti.v1i03.30.
14- Wu, J., Mayer, A., & Li, R. (2020). Integrated imaging and molecular analysis to decipher tumour microenvironment in the era of immunotherapy.. Seminars in cancer biology. https://doi.org/10.1016/j.semcancer.2020.12.005.
15- Grand View Research, AI In Oncology Market Size, Share & Trends Analysis Report, 2024 – 2030.